A 17 yo thin built girl presents to the emergency department with cough since 2 days, abdominal pain, nausea and vomiting since evening. Patient had an episode of fever a day ago.
Abdominal pain: Diffuse, dull aching no aggravating or relieving factors, severity- 8/10 on VAS
Vomiting: Multiple episodes with food particles, Non bilious, No blood, associated with nausea
On further questioning, the patient told she is having palpitations. She also told that she is feeling weak and fatigued since last 2 days.
Patient is a school going girl and comes to home straight after school and seldom leaves the house afterwards. There is no significant prior medical history, no known allergies and the patient is not taking any medications.
Vitals: HR 130 / BP 100/60 / T35.7 / RR 24 / SpO2 98% on room air.
Physical Examination
General: Drowsy, pale.
HEENT: Non-icteric, MM dry.
Pulmonary: Tachypnea.
Cardiovascular: Tachycardia, regular, no murmur.
Abdomen: No peritonitis, mild diffuse abdominal tenderness, thin
USG Abdomen: Normal except Mild volume depletion
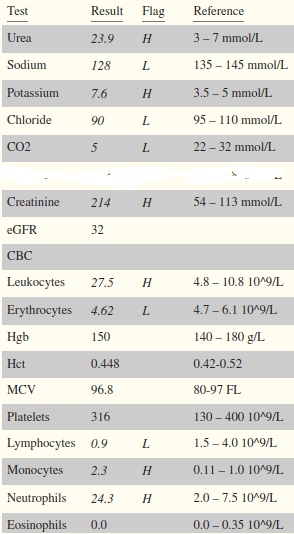
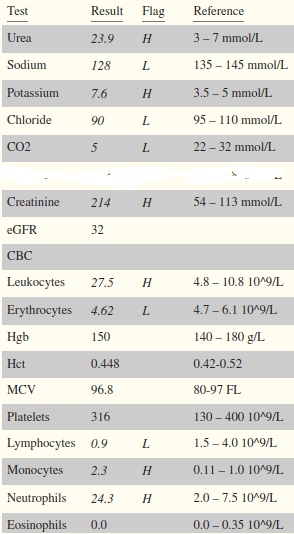
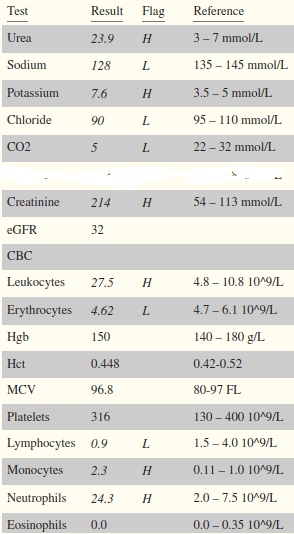
Meanwhile, you order CBC, LFT, KFT and Electrolytes
How will you further evaluate the patient?
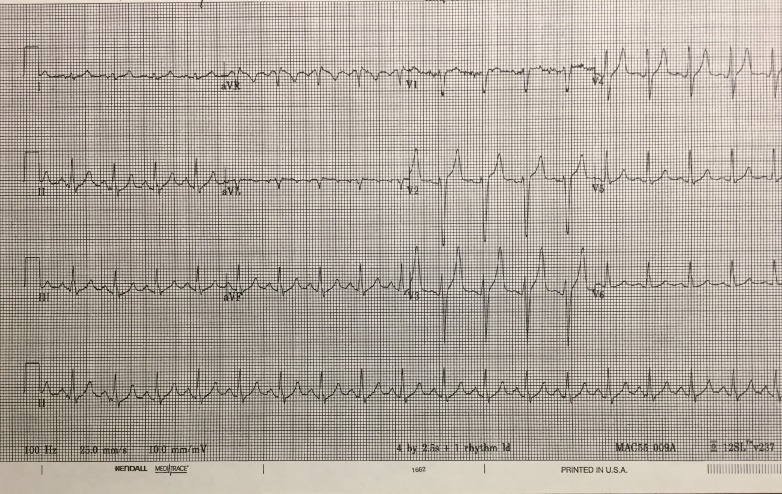
X-Ray abdomen came out to be normal. You next do an ECG to evaluate for palpitation and abdominal pain.
While you are looking at the ECG, patient’s mother comess to you and tells you that her daughter is feeling drowsy and is acting confused. You check respiratory rate which is 25 breaths/min.
You quickly do an RBS which shows- 466 md/dl.
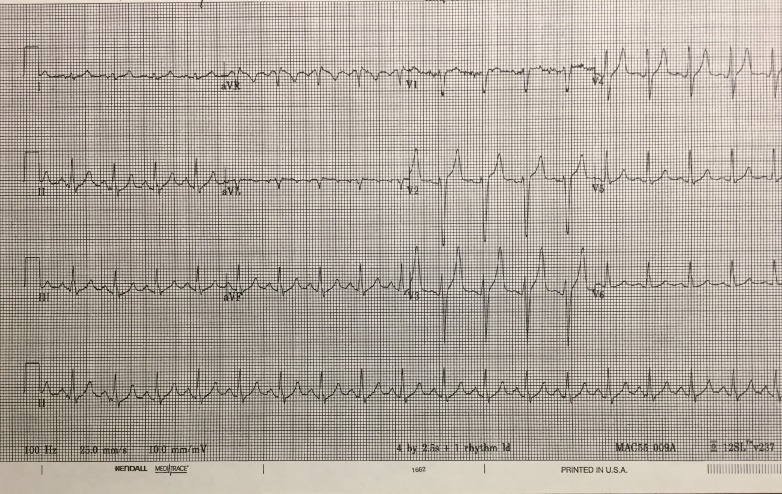
You do an ECG to evaluate for palpitation and abdominal pain.
While you are looking at the ECG, patient’s mother comess to you and tells you that her daughter is feeling drowsy and is acting confused. You quickly do an RBS which shows- 486 md/dl.
What would you like to do next?
Your senior intervenes and quickly administer calcium gluconate and scolds you. He says that the patient is showing signs of dangerous hyperkalemia so cardioprotection is our priority. What would you do next?
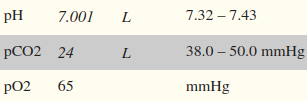
You found that in the patient’s left hand, the ulnar circulation is not patent though it is fine in right. You do the ABG from the right Radial artery where the allen’s test is normal. Meanwhile, all the reports arrive.
You need to start IV Fluids according to the dehydration status of the patient. Dehydration is assesed by sodium content of the serum. Assuming, Serum sodium concentration decreases by 2.4 mEq/l for every 100 mg/dl increase in glucose concentration. Assess the dehydration status of the patient and administer the right IV Fluid.
Sodium= 128 mmole/L and Glucose= 486 mg/dl.
As soon as you are starting to do the ABG, your friend who is watching you, reminds you the consequence of doing an ABG without checking the patency of circulation of hand. If the ulnar circulation is not patent, arterial thrombosis after ABG can lead to dangerous ischemia, gangrene and necrosis.
You now do an Allen’s test and then perform ABG. Meanwhile, all the reports arrive.
You need to start IV Fluids according to the dehydration status of the patient. Dehydration is assesed by sodium content of the serum. Assuming, Serum sodium concentration decreases by 2.4 mEq/l for every 100 mg/dl increase in glucose concentration. Assess the dehydration status of the patient and administer the right IV Fluid.
Sodium= 128 mmole/L and Glucose= 486 mg/dl
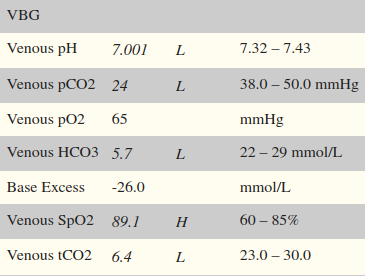
You do the VBG. Meanwhile, all the reports arrive.
You need to start IV Fluids according to the dehydration status of the patient. Dehydration is assesed by sodium content of the serum. Assuming, Serum sodium concentration decreases by 2.4 mEq/l for every 100 mg/dl increase in glucose concentration. Assess the dehydration status of the patient and administer the right IV Fluid.
Sodium= 128 mmole/L and Glucose= 486 mg/dl
Before you start infusing saline, your senior warns you to check the corrected sodium rather than the sodium in reports. You check the corrected sodium and it comes out to be higher than 135 mmole/l which warrants for administration of 0.45% saline. You start it at 250 to 500 ml/hr. Meanwhile, ABG reports arrive. How will you manage the patient next?
Explain Type Your senior who is monitoring you stops you and explains- bicarbonate is only tried if pH falls below 6.9 and KCl shouldn’t be started when blood potassium levels are already above 7. Also, patient doesn’t need pressors as the paient is not in shock. You then start IV Regular Insulin at 0.14 Units/kg/hr after thanking your senior to enlighten you.
Your senior then asks you an interesting qs. He asks, in fact- Why not? Why don’t we consider giving bicarbonate in patients admitted to ICU unless the patient is in severe acidosis? What damage could it possibly do? He also asks you if you have anything better than sodium bicarbonate to give to patients(in ICU setting), if yes, tell what it is and Why?
Explain Type You start IV Regular Insulin at 0.14 Units/kg/hr.
Your senior then asks you an interesting qs. He asks, in fact- Why not? Why don’t we consider giving bicarbonate in patients admitted to ICU unless the patient is in severe acidosis? What damage could it possibly do? He also asks you if you have anything better than sodium bicarbonate to give to patients(in ICU setting), if yes, tell what it is and Why?
Before you start infusing saline, your senior warns you to check the corrected sodium rather than the sodium in reports. You check the corrected sodium and it comes out to be higher than 135 mmole/l which warrants for administration of 0.45% saline. You start it at 250 to 500 ml/hr. Meanwhile, VBG reports arrive.
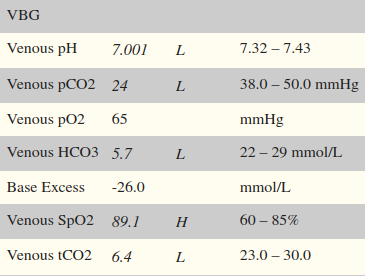
You start 0.45% saline at 250 to 500 ml/hr. Meanwhile, ABG reports arrive. How will you manage the patient next?
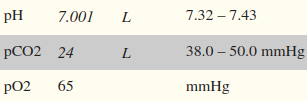
You start 0.45% saline at 250 to 500 ml/hr. Meanwhile, VBG reports arrive. How will you manage the patient next?
You keep monitoring serum glucose and K+ levels. After a series of measurements eventually the following results come.
glucose= 190 mg/dl and K+= 4.5 mmole/l Choose the correct path from the following.
Explain Type You take a look at all the reports which seemed to be more or less fine and you are thinking of discharging the patient.
Your junior disagrees and says the patient’s condition is not improving. He explains that the bicarbonate levels seen in the reports are around 9 consecutively in last few reports and pH is around 7.1 which means that the DKA is not resolving.
How will you explain your junior what is happening actually and why you think the patient is improving? Also mention a better marker to check for the resolution of DKA in such cases.
Now you want to discharge the patent as the patient is stable now and all the labs are showing improvement.
You go away for a few hours confident that the patient will be alright.
When you were away, patient suffered convulsions which were later found to be due to hypoglycemia. You were scolded heavily by your seniors and were remmoved from the case :(
You scored 0 points.
Thank you for completing the case!
You go away for a few hours confident that the patient will be alright.
When you were away, patient suffered fatal arrhythmia which were later found to be due to hypokalemia. You were scolded heavily by your seniors and were remmoved from the case :(
You scored 0 points.
Thank you for completing the case!
Patient had another episode of Diabetic ketoacidosis and returned to the hospital emergency. She was stabilised again and then was sent home. This time, the patient was transitioned to subcutaneous insulin before being sent home.
You scored 0 points.
Thank you for completing the case!
The patient was discharged and case was closed.
Patient returned to her normal life pretty soon and was fine in subsequent follow ups.
Hope you enjoyed the case!! References: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5491337/#REF3 Good Job Doctor!!
You scored 0 points.
Thank you for completing the case!